Burden and risk-factors of TB
Tuberculosis (TB) is a major public health concern even in current era causing 1.57 million deaths annually. The World Health Organization has set a target of eliminating TB by 2030, whereas India has promised to end it by the year 2025. Despite the promise, India still accounts for more than one-fourth of the cases and ~36% of global mortality. The heavy TB burden in India is an aftermath of multiple prevalent risk factors like wide-spread under-nutrition, alcohol & tobacco use, diabetes and human immunodeficiency virus infection. To add to the turmoil, over-crowding is also a major problem in India due to growing population. This has impacted TB transmission and incidence of latent TB infections (LTBI). In Indian context as per a recent study, almost 71% household contacts have baseline LTBI. Approximately, 5-10% of those with LTBI will develop active TB subsequently with majority developing in first two years of contact. If an active TB disease is left untreated, each of those cases can infect another 10-15 individuals every year facilitating this chain, which hurdles the TB elimination strategies.
Challenges in TB elimination
- Notification gap: We have a huge notification gap in TB cases leading to many undetected cases increasing the transmission potential and risk of tuberculosis in our country. These cases may also add to difficult to treat cases with poor outcome causing more mortality and morbidity in TB patients.
- Drug Resistant TB (DRTB) challenge & success rate: Similarly, DRTB also having huge burden and notification gap between estimated and diagnosed cases in our setting. The success rates are also relatively lower success rate among these patients which is often attributed to poor compliance due to injectable, longer regimen with multiple tablets and more serious side effects.
- Higher burden of risk factors: In Indian setting still, undernutrition continues to be rampant which have the highest attributable fraction of risk of TB. This further explains the rationale of the emerging concept of “Food as vaccination for TB”. Famous ‘Reducing Activation of Tuberculosis by Improvement of Nutritional Status’ (RATIONS) trial which was published recently also sheds light on the same issues.
Strategies to tackle TB using TB Preventive Therapy (TPT)
TPT has been shown to be an effective strategy for preventing TB infection and disease, particularly in high-risk groups. Previously the focus of TPT was among children less than 5 years and people living with HIV/AIDS (PLHA). Recent revision has expanded TPT regimen to household contact of any age to improve coverage. However, the proportion of eligible individuals initiated on TPT is much lower than national strategic plan targets.(Fig.1) To determine whether individuals and groups with a high risk of contracting TB are eligible for TPT, it is necessary to first rule out active TB through the use of available tests. Subsequently, individual may be tested for LTBI using tuberculin skin test (TST) or interferon gamma release assay (IGRA) and started on TPT. However, TPT shouldn’t be deferred in the absence of these.
Both TST and IGRA works on the principle of type-IV hypersensitivity and each has its own pros and cons. IGRA is highly sensitive and specific test which can be used in prior BCG vaccinated individuals, whereas TST is less costly which doesn’t require sophisticated lab and infrastructure. The TPT regimen which was followed commonly was six monthly daily isoniazid regimens. However, in order to improve compliance recently Isoniazid plus rifapentine was also introduced which is weekly regime for three months.
By reducing the incidence of TB, TPT can help to break the chain of TB transmission and ultimately contribute to the overall reduction of TB burden. TPT usage is quintessential in high-risk groups where the conversion risk of LTBI to active disease is high. For instance, in the case of HIV coinfection, the risk is 16-21 times higher, and in individuals with other immune-compromised statuses such as diabetes, the risk is 3-4 times higher6.
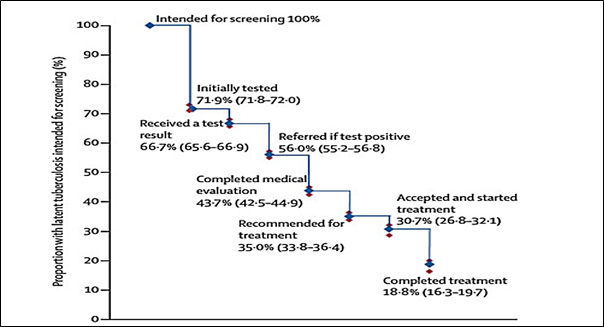
| Fig.1. Losses and drop-outs at each stage of cascade of care in LTBI. Ref: Central TB Division, Ministry of Health & Family Welfare. Guidelines for Programmatic Management of Tuberculosis Preventive Treatment in India. New Delhi. |
Research and Innovations in TPT
One of the major pillars of the End TB Strategy is collaborative research and innovation. TPT can play a role in this pillar by providing a platform for research and innovation in TB prevention. There is ongoing research into new drugs and regimens for TPT, as well as new methods for identifying people who are at high risk of TB infection or disease. Recent guidelines give TPT regimen for drug-resistant TB contact too. Also, there is piloting of newer skin test named “CyTB” to detect LTBI. In addition, we have “the Prevent TB app” by world health organisation to aids in enrolling, monitoring, and managing TPT making a comprehensive TB surveillance system for India.
Challenges and way forward
Despite the advances in TB care still there are considerable losses in cascade of care before the initiation of TPT (Fig. 16). The global statistics point out that around 20% of eligible individuals are only completing the treatment. The data for Indian sub-continent shows even less coverage in TPT implementation. Strengthening of the entire continuum of care is an essential step to march towards TB elimination.
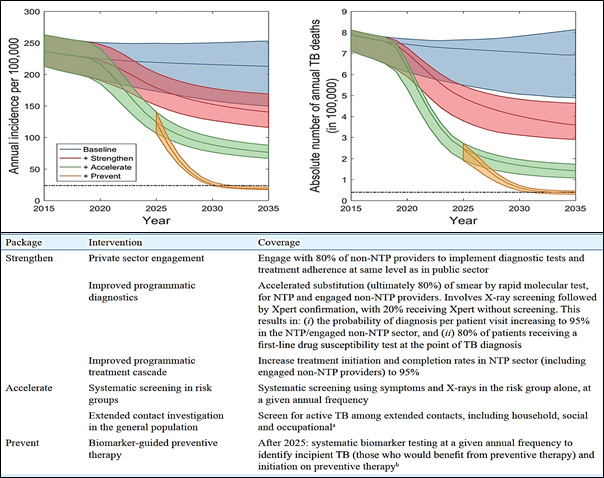
| Fig.2. Strategies for ending tuberculosis in South-East Asian region: A modelling approach.
Ref: Arinaminpathy N, Sharma M, Swaminathan S, et al. Strategies for ending tuberculosis in the South-East Asian Region: A modelling approach. Indian J Med Res. 2019;149:517–27. |
Further modelling studies by various institutes also recommend multiple packages to accelerate TB elimination(Fig. 2). While challenges remain, the adoption of TB preventive therapy, along with strengthened surveillance and innovative approaches, can pave way for TB elimination by 2025.