World Neglected Tropical Disease Day is celebrated every year on 30 January 2025 with the 2025 theme being “Unite, Act, and Eliminate.” Lymphatic filariasis (LF) is one of the neglected Tropical diseases (NTD). According to the World Health Organization (WHO), an estimated 120 million people in 72 countries are infected, with over 40 million suffering from chronic disability. The disease is endemic in tropical and subtropical regions, particularly in Africa, South Asia, Southeast Asia, and parts of Latin America and the Pacific Islands.
Lymphatic Filariasis (LF), commonly known as elephantiasis, is a disabling and disfiguring parasitic disease caused by Wuchereria Bancrofti (most commonly), Brugia malayi, and Brugia timori. The disease is transmitted to humans through mosquito vectors, including Anopheles, Culex (most commonly), and Aedes species. It primarily affects the lymphatic system, leading to severe swelling of the limbs, genitalia, and other body parts.
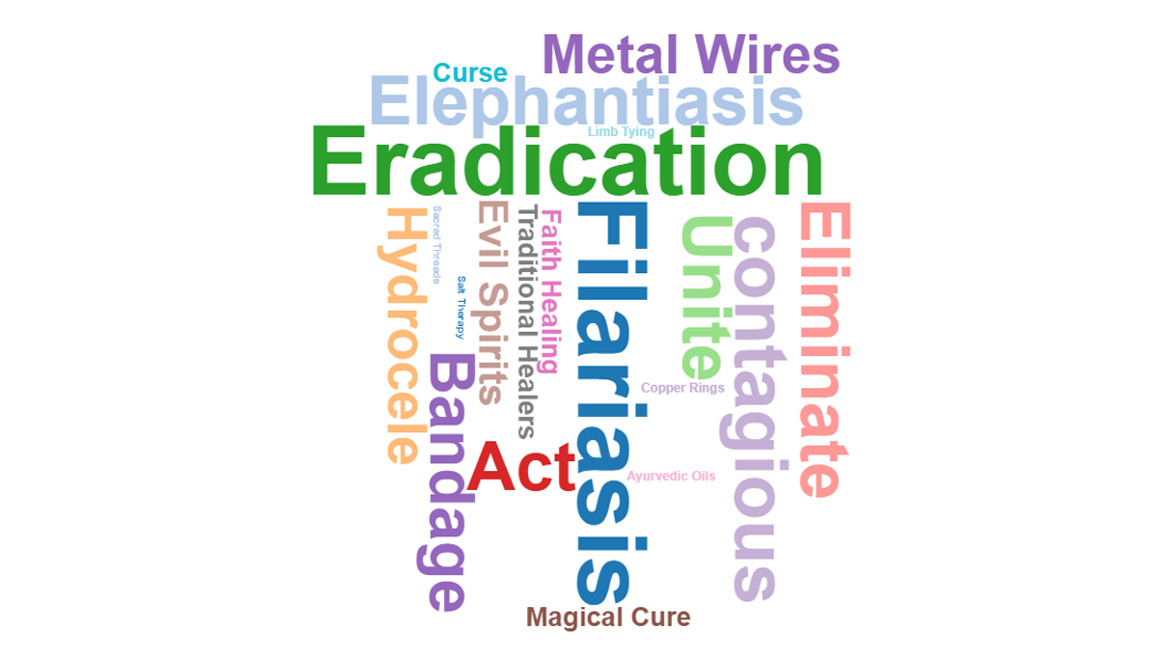
Although LF is usually not fatal, its physical and psychological impact can be devastating. The disease causes social stigma, economic hardships, and rising healthcare expenses, ultimately keeping affected individuals trapped in a cycle of poverty. With global elimination efforts led by WHO through the Global Programme to Eliminate Lymphatic Filariasis (GPELF), mass drug administration (MDA) campaigns are being implemented to interrupt transmission and manage morbidity. However, challenges such as low compliance, misinformation, and healthcare infrastructure limitations continue to hinder eradication efforts. Despite a lot of efforts by the government to eliminate lymphatic filariasis but there are lot of prevailing myths related to lymphatic filariasis and its management.

These myths and false practices are-
Debunking the myth of wire-tying
Lymphoedema in LF occurs due to damage to the lymphatic system by filarial parasites. The swelling is caused by fluid accumulation, and tying wires around the limb does not remove the accumulated fluid or kill the parasite.
Herbal or Traditional Remedies Can cure LF
Certain herbal treatments may provide temporary relief from symptoms like itching or swelling but they do not kill the parasitic worms that cause LF. Some traditional healers claim to “remove” the disease by cutting open the swollen area and draining fluid, which can lead to serious infections and complications. The most effective treatment remains antifilarial medications such as Diethylcarbamazine (DEC), Albendazole, and Ivermectin.
Mass Drug Administration (MDA) Pills Cause Sterility
One of the most harmful myths about LF prevention is the belief that MDA medications cause infertility. Men refuse to take antifilarial drugs due to fear that they will lose their reproductive ability. This false belief reduces drug uptake, leading to continued transmission of the parasite. The reality is that MDA medications are safe, approved by WHO, and essential for breaking the cycle of infection.
Hydrocelectomy in LF causes sterility
Many patients with hydrocele hesitate to seek medical attention or disclose their condition due to shame, embarrassment, or fear of social stigma. Many individuals avoid hydrocelectomy due to the fear of sterility, leading to prolonged suffering, social stigma, and reduced quality of life. The surgery is performed to relieve discomfort, improve mobility, and prevent further complications.
Hot Compression
In many rural and endemic areas, patients with swollen legs, arms, or scrotum due to LF believe that applying heat will reduce their symptoms and provide long-term relief from pain and discomfort. While heat may provide temporary relief, these practices are scientifically unfounded and can lead to serious complications.

Walking Barefoot cures Lymphatic Filariasis
Walking barefoot is a common habit in many rural and endemic areas, but for Lymphatic Filariasis (LF) patients, it can lead to severe complications.
Conclusion
Lymphatic Filariasis (LF) is a neglected tropical disease that remains a significant public health issue, especially in tropical and subtropical regions. Despite ongoing global efforts to eliminate it, misconceptions and false beliefs continue to impede progress. Superstitions, reliance on traditional remedies, and fear of medical treatments prevent timely diagnosis and proper management. Mass Drug Administration (MDA) is a safe and essential strategy to break the cycle of transmission. Hydrocelectomy does not cause sterility and should not be avoided due to fear or stigma.
To achieve WHO’s goal of eliminating LF as a public health problem, it is crucial to improve drug compliance through education campaigns, address myths and cultural beliefs that discourage treatment promote healthy practices, such as limb hygiene and mosquito control
Reduce social stigma by promoting community awareness.