When it comes to early childhood health, much of the attention has traditionally been on mothers. However, a growing body of research shows that fathers play an equally crucial role in shaping their child’s health and development, starting even before conception (Burgess, 2017) . From influencing sperm quality to providing emotional and financial support, paternal health and behaviours have long-term impacts on pregnancy outcomes and child well-being. This blog explores the critical role of fathers in child health, the often-overlooked impact of paternal well-being, and the importance of integrating fathers into public health strategies.
Understanding the Importance of Paternal Health
The early years of life, especially from conception to two years of age, are crucial for cognitive, emotional, and physical development (World Health Organization [WHO], 2021). While maternal health is well-documented, research suggests that paternal health significantly affects pregnancy outcomes, child development, and long-term health trajectories (Soubry, 2018).
Preconception Health: Fathers’ Role in Healthy Beginnings
Preconception health refers to the health status of both parents before conception. While much emphasis is placed on maternal nutrition, chronic disease management, and lifestyle choices, fathers’ health is equally vital.
Impact on Sperm Quality and Child Development
Paternal factors such as obesity, smoking, alcohol consumption, and exposure to environmental toxins can impair sperm quality, affecting fertilization and increasing the risk of miscarriage, congenital anomalies, and preterm birth. Additionally, research suggests that paternal obesity can alter sperm DNA methylation, potentially predisposing children to metabolic disorders (Glynn et al., 2016).
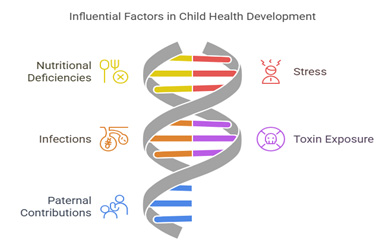
Epigenetics: The Hidden Influence of Paternal Health
Epigenetics—the study of how behaviours and environment influence gene expression—highlights how paternal health can affect offspring beyond direct genetic inheritance (Soubry, 2018) . Stress, poor diet, and toxin exposure can lead to epigenetic changes in sperm, altering gene expression in the developing foetus. For example, studies have linked paternal malnutrition to increased risk of metabolic and cardiovascular diseases in children, emphasizing the importance of a father’s well-being even before conception (Feldman, 2015).
Beyond Conception: Fathers’ Role in Pregnancy and Early Childhood
While much focus is placed on maternal prenatal care, fathers’ physical and mental health during pregnancy also significantly impact child outcomes (Alio et al., 2010). Fathers contribute in multiple ways, including emotional support, stress management, and shaping a positive household environment (Alio et al., 2010).
1. Mental Health Matters
Fathers’ mental health before and after a child’s birth plays a crucial role in family dynamics. Paternal depression and high-stress levels have been associated with behavioural and emotional issues in children. Fathers experiencing mental distress are less likely to engage in positive parenting behaviours, which can negatively impact child development. Addressing fathers’ mental well-being through counselling, peer support, and awareness campaigns is essential for fostering healthy family relationships.
2. Role Modelling Healthy Behaviours
Children often adopt the lifestyle habits of their parents. Fathers who maintain a nutritious diet, exercise regularly, and avoid harmful habits such as smoking and excessive alcohol consumption set a positive example for their children. Conversely, an unhealthy paternal lifestyle can contribute to childhood obesity, respiratory illnesses, and long-term health risks.
3. Involvement in Infant Care: The Case for Kangaroo Care
Skin-to-skin contact, known as Kangaroo Care, is a proven method to promote bonding, regulate a newborn’s body temperature, and support healthy growth. Traditionally associated with mothers, fathers can also engage in Kangaroo Care to strengthen early emotional connections with their newborns. Active involvement in newborn care fosters confidence in parenting and contributes to improved child development outcomes.
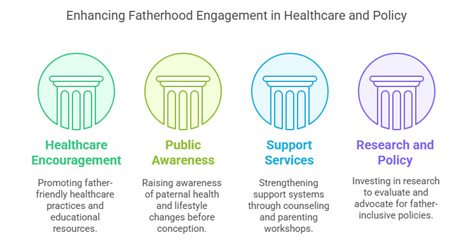
Closing the Gap: How to Integrate Fathers into Child Health Strategies
Despite the overwhelming evidence of paternal influence on child health, many public health initiatives still focus primarily on maternal well-being. Addressing this imbalance requires systemic changes in healthcare, policy, and community support.
1. Encouraging Father-Inclusive Healthcare (Burgess, 2017)
- Promote father-friendly prenatal visits and birth classes.
- Provide targeted educational materials for expectant fathers.
- Advocate for workplace policies that support paternity leave and early childcare involvement.
2. Raising Awareness Through Public Health Campaigns (Ramchandani et al., 2013)
- Highlight the importance of paternal health in reproductive planning.
- Encourage lifestyle changes among men before conception.
- Address paternal mental health as part of perinatal care initiatives.
3. Strengthening Support Services for Fathers (WHO, 2021)
- Offer counselling and peer support groups for expectant and new fathers.
- Develop parenting workshops focused on early childhood care and emotional bonding.
- Create online resources and community networks to support active fatherhood.
4. Investing in Research and Policy Development (Soubry, 2018)
- Conduct long-term studies on paternal health influences on child development.
- Evaluate the effectiveness of father-inclusive interventions.
- Advocate for policy changes to recognize and support fathers’ roles in reproductive and child health programs.
Conclusion: A Call to Action for Inclusive Parenting
Fathers are not just secondary caregivers—they are essential contributors to their child’s health, beginning before conception and continuing through early childhood. By shifting the narrative to recognize and support paternal health, we can create more comprehensive strategies that benefit not only children and families but society as a whole. It is time to move beyond traditional maternal-centric approaches and embrace an inclusive model where fathers are actively involved in shaping the future generation’s well-being.
References:
- Burgess, A. (2017). “The role of fathers in child development: An evidence review.” Fatherhood Institute. [Available at: https://www.fatherhoodinstitute.org/]
- Wan, M. W., et al. (2020). “Paternal mental health and child development: Why it matters.” Infant Mental Health Journal, 41(3),
- Feldman, R. (2015). “The adaptive human parental brain: Implications for children’s social development.” Trends in Neurosciences,
- Glynn, L. M., et al. (2016). “Paternal programming of offspring development.” Biological Psychiatry, 80(10)
- World Health Organization (WHO). (2021). “Fathers’ roles in early childhood development.” [Available at: https://www.who.int/]
- Alio, A. P., et al. (2010). “The impact of paternal involvement on foetal and infant health outcomes in the United States.” Maternal and Child Health Journal, 14(5).




